Overview
Pelvic health physiotherapy is a specialist area of physiotherapy that focuses on problems occurring around the abdomen and pelvis. We focus on restoring strength, function and movement within the pelvic area. We are specialist physiotherapists and we have undergone further training into this area of the body.
We treat women over the age of 18 with:
- Stress incontinence – urinary leaking with certain activities.
- Overactive bladder – having a sudden desire to go to the toilet immediately with possible leaking of urine before reaching the toilet. There may be a need to visit the toilet more frequently than normal.
- Mixed urinary incontinence – a combination of stress incontinence and overactive bladder.
- Small to moderate prolapse of the front and/or back vaginal wall(s) – weakening of the support structures that support the vagina, resulting in bulging of the pelvic organs into the vagina.
- Pain related pelvic floor dysfunction e.g. vaginismus and vulvodynia.
- Post natal pelvic girdle pain, perineal trauma and diastasis rectus abdominus.
- Faecal incontinence – leakage of faeces and wind.
- Obstructive defecation – difficult emptying the bowel, which may or may not be associated with constipation.
- Pelvic girdle pain-pain around the pelvis, hips and lower back in pregnancy.
Click the below buttons to explore our pelvic health resources and information
Physiotherapy and Women's Health Self-referral
If you are an adult registered with a Mid Essex GP practice, you can now self-refer to physiotherapy for any musculoskeletal, or Women’s Health related issues subject to the local NHS service criteria.
Pelvic organ prolapse
Pelvic organ prolapse is when either the bladder, bowel or uterus descend into the vagina. It can happen to one or more of the pelvic organs. This is a common problem that happens in women and research suggests that 1 in 2 women over the age of 50 will have a prolapse. It is also common in younger women post pregnancy and childbirth. It can also affect women who have not been pregnant or given birth. Some women will have no symptoms and others may feel a bulge sensation or a tampon in the wrong place or a heaviness in the vagina.
Pelvic organ prolapse is not a life-threatening condition, and not all prolapses get worse; some may improve. If you have been told that you have a pelvic organ prolapse you may have the following choices:
- do nothing and wait and see how your symptoms change
- adopt good bladder and bowel habits
- Avoid and/or manage any constipation and straining
- Perform the ‘knack’ where you tighten the pelvic floor during activities that bring on your symptoms e.g.: coughing, sneezing, lifting, pushing, pulling, sit to stand
- Sit down/rest if you are getting uncomfortable when standing/walking
- make lifestyle changes to reduce the downward pressures through your pelvis, particularly if some of your existing activities make your symptoms worse e.g. weight loss, trying to avoid or reduce the amount of lifting you do and avoid straining to open your bowels
- improve the strength of your pelvic floor muscles to increase the vaginal support
- try a vaginal pessary which will support the vaginal wall
- speak to a gynaecologist about the possibility (or option) of surgery. You may choose to do nothing if your prolapse is not bothersome.
However, research suggests you can prevent your prolapse getting worse by doing your pelvic floor muscle exercises regularly.
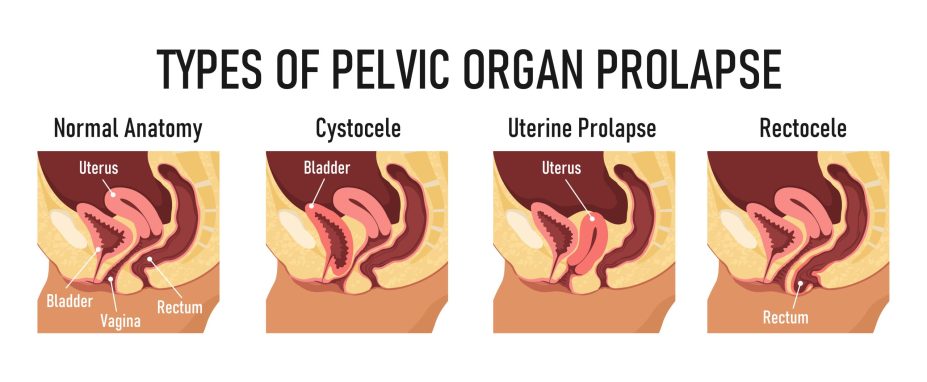
An anterior wall prolapse or a cystocele is where a descended bladder pushes the front wall of the vagina down. This may cause increased urinary frequency and it can also cause urinary incontinence.
A uterine prolapse is where the uterus drops down into the vagina. The cervix will be felt lower down in the vagina.
A posterior wall prolapse or rectocele is where the rectum drops forward into the back wall of the vagina. This can cause the perineum to become lax, and it may cause problems with opening bowels.
We would often teach pelvic floor muscles exercises to our patients with pelvic organ prolapse. Strengthening these muscles can help to support the pelvic organs more and lessen the symptoms of a prolapse. It will take several months of pelvic floor strengthening to notice the difference.
It is also important to identify other factors which may be worsening the prolapse. Risk factors include being overweight, heavy lifting, constipation and having a chronic cough. There is no evidence that any exercise or high impact activities will worsen a prolapse. Physiotherapists can help you to work on reducing these risks to reduce the strain on the prolapse.
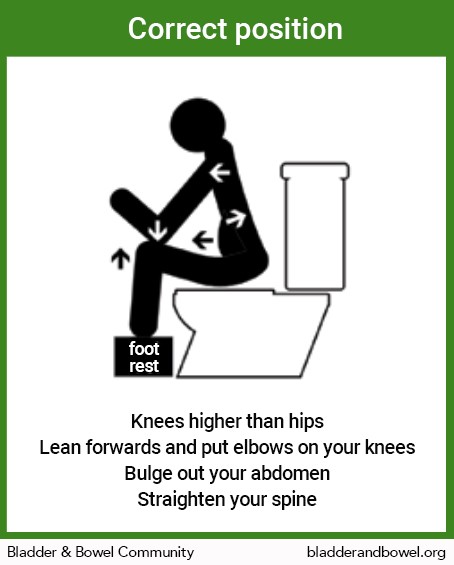
Optimal bowel opening position pictures
Useful Links
- Pelvic Organ Prolapse: A guide for women – Booklet for women who have or feel they have symptoms associated with a pelvic organ prolapse.
- The British Society of Urogynaecology (BSUG) – is a good resource for further information

