Overview
There are many causes of multiple joint pain. The possible causes will partly depend on your age and the causes for multiple joint pain in children are different to the causes in adults.
Multiple joint pain may be completely harmless and only temporary problems although some causes may require medical investigations and a referral for you to see a specialist to confirm a diagnosis including long-term treatment in some cases.
Sometimes, multiple joint pain may develop alongside other health problems which may be connected and require different forms of management.
The term ‘arthritis’ is most commonly used to explain the cause of pain, swelling and stiffness in joints although arthritis is NOT a single condition and there a several different types.
For more information, read the other sections and watch this short video for further support.
Type of Multiple Joint Pain
Osteoarthritis is the most common type of arthritis and it is estimated to effect approximately 9 million people in the UK. The parts of the body most commonly affected are your knees, hips, hands, feet and back.
It is a normal age-related process resulting in pain and stiffness of one or multiple joints, usually worse after prolonged rest or activity and for the first 30 minutes in the morning.
Osteoarthritis mainly affects people over the age of 55 and is more common in women.
The early stages of osteoarthritis can happen without causing much pain or problems and even the later stages of the condition can be effectively self-managed with physical activity, weight loss and regular exercise.
The severity of changes seen on X-ray or scan does not always correlate with the amount of pain or problems you are experiencing.
Only a small proportion of people with osteoarthritis require surgery in severe cases, mainly for hips and knees. However, most people can manage the condition using conservative measures.
This comprehensive information booklet explains the condition in more detail including hints and tips on how to manage your osteoarthritis in daily life:
Osteoarthritis
For advice on managing osteoarthritis of specific joints, click on Self Help and select the part of the body you’re having pain with.
Watch this short-animated video by Versus Arthritis to find out more about what osteoarthritis is, what the treatment options are and what you can do to help yourself.
For useful exercises to carry out at home to manage your osteoarthritis, Click Here.
For help with weight loss and increasing physical activity levels, visit Essex Wellbeing Service and self-refer.
Rheumatoid arthritis is a type of inflammatory arthritis that causes pain, swelling and stiffness in your joints, usually affecting the hands, feet and wrists. It affects around 400,000 adults in the UK and although it can affect people of any age, most are diagnosed between the ages of 40 and 60.
It is known as an auto-immune condition which is where the immune system, your body’s own natural self-defence system, gets confused and attacks your body’s healthy tissues. In rheumatoid arthritis, the main way it does this is by creating inflammation in your small joints usually.
Watch this short-animated video by Versus Arthritis to find out more about what rheumatoid arthritis is, what the treatment options are and what you can do to help yourself.
The earlier the condition is diagnosed, the sooner you can start treatment and the more effective it is likely to be, so Click Here for more information on common symptoms of rheumatoid arthritis and what medical investigations are needed to confirm the diagnosis.
For people who have already been diagnosed with rheumatoid arthritis, Click Here for a comprehensive information booklet explaining the condition in more detail.
As well as receiving the appropriate medical treatment from your GP or specialist, it is also important to have an active and healthy lifestyle as this can help to reduce joint pain and stiffness related to rheumatoid arthritis. For further support with this, visit Essex Wellbeing Service and self-refer.
Psoriatic arthritis is a type of inflammatory arthritis that causes pain, swelling and stiffness in and around your joints and sometimes your spine. It can affect people of any age but often begins when someone is in their 30’s. It usually affects people who already have a skin condition called psoriasis and it’s estimated that around one in five people with psoriasis will develop psoriatic arthritis.
Both psoriatic arthritis and psoriasis are auto-immune conditions which is where the immune system, your body’s own natural self-defence system that protects you from illness and infection, gets confused and attacks your body’s healthy tissues. In psoriatic arthritis, the main way it does this is by creating inflammation in your joints, spine or tendons and ligaments around the joint, especially in your heel and foot.
Watch this short-animated video by Versus Arthritis to find out more about what psoriatic arthritis is, what the treatment options are and what you can do to help yourself.
The earlier the condition is diagnosed, the sooner you can start treatment and the more effective it is likely to be, so Click Here for more information on common symptoms, diagnosis and treatment of psoriatic arthritis.
For people who have already been diagnosed with psoriatic arthritis, Click Here for an information booklet explaining the condition in more detail.
As well as receiving the appropriate medical treatment from your GP or specialist, it is also important to have an active and healthy lifestyle as this can help to reduce pain and stiffness related to psoriatic arthritis. For further support with this, visit Essex Wellbeing Service and self-refer.
Reactive arthritis, formerly known as Reiter’s Syndrome, is a type of inflammatory arthritis that causes you to have extremely painful, swollen joints and can make you feel very tired. It starts after you’ve had an infection somewhere else in the body, such as a tummy bug or throat infection, and the most common joints to be affected are your knees and ankles.
Unlike other types of inflammatory arthritis, for many people reactive arthritis lasts a relatively short period of time and it usually clears up within 6 months without causing any lasting joint problems.
For more information on common symptoms, diagnosis and treatment of reactive arthritis – Click Here.
This booklet provides further information and answers to your questions about reactive arthritis.
Reactive Arthritis
Ankylosing spondylitis, also known as axial spondyloarthritis, is a type of inflammatory arthritis that mainly affects your back as a result of inflammation in the spine causing back pain and stiffness, especially in the early morning lasting longer than 30 minutes and then eases through the day or with activity.
It usually starts in people who are in their 20’s and it is three times more common in men than in women with approximately 1 in 1000 people in the UK develop ankylosing spondylitis. Although it mainly affects your back and neck, it can also cause pain elsewhere in your body, including in your hips, shoulders and feet.
Watch this short video explaining ankylosing spondylitis and how it can affect your life.
We don’t know exactly what causes ankylosing spondylitis and although there is not a cure, there are a number of treatments that can slow the condition down and reduce pain and stiffness.
For more information on common symptoms, diagnosis and treatment of ankylosing spondylitis – Click Here.
This booklet provides further information and answers to your questions about ankylosing spondylitis.
As well as receiving the appropriate medical treatment from your GP or specialist, it is also important to have an active and healthy lifestyle as this can help to reduce back pain and stiffness related to ankylosing spondylitis. For further support with this, visit Essex Wellbeing Service and self-refer.
See Self Help for general advice and exercises for back pain.
Gout is the most common type of inflammatory arthritis which affects men more than women. It is temporarily a very painful type of arthritis caused by crystals that form in and around the joint.
It usually affects the big toe although other joints can be affected including ankles, knees, elbows, wrists and fingers. During an attack of gout, the affected joint(s) will become very painful, tender, red, hot and swollen. The attack usually settles after approximately five to seven days, but it can last longer.
To find out if you may be at increased risk of developing gout – Click Here.
Click Here for immediate advice and when to see your GP if you suspect you have gout and the do’s and don’ts for managing an attack as well as preventing it coming back.
Gout occurs if you have high levels of urate in your blood, but having urate in your blood doesn’t necessarily mean you will develop the condition. Urate crystals can slowly start forming if the urate levels remain too high and build up in and around joints and occasionally under your skin.
For more information on common symptoms, causes, diagnosis and treatment of gout – Click Here.
This booklet provides further information and answers to your questions about gout.
As well as receiving the appropriate medical treatment from your GP, it is also important to look at other factors that might be contributing to your gout and future attacks including being overweight. For help with weight loss and making other healthy lifestyle changes, visit Essex Wellbeing Service and self-refer.
Juvenile idiopathic arthritis (JIA) is a type of inflammatory arthritis that affects children under the age of 16, slightly more common in girls, causing inflammation in one or more of your joints.
There are different types of JIA and symptoms and outlook vary between the different types. The most common symptoms are painful, swollen or stiff joints that last longer than 2 weeks often accompanied with tiredness and a fever that keeps returning.
If you think that you or someone you know may have JIA, book a GP appointment as soon as possible.
For more information on symptoms, causes, types, diagnosis and treatment of JIA – Click Here.
Joint hypermobility is very common, especially in children, and simply means that you can move some or all of your joints more than most people can and is NOT a type of arthritis. It is often referred to as being ‘double jointed’ and you may have been aware from an early age that your joints were more flexible than other people’s.
Hypermobility itself is not a medical diagnosis and most people have no symptoms or problems, with it actually being an advantage in some sports, playing a musical instrument and dance.
However, some people with hypermobile joints may have symptoms including joint or muscle pain and some level of fatigue. You may also find that your joints are prone to injury or even dislocation. If you do have these symptoms then you may have joint hypermobility syndrome.
For more information on symptoms, causes, diagnosis and treatment of joint hypermobility – Click Here.
This booklet provides further information and answers to your questions about joint hypermobility.
Unless you have other associated symptoms with joint hypermobility such as abdominal or chest pain, palpitations, bladder incontinence or feeling faint when standing up, it is unlikely you’ll need any medical help and the best way of managing it is with exercises to strengthen the muscles around the hypermobile joints and pacing your activity if necessary. Physiotherapy can be very beneficial if you’re still having symptoms and problems.
For help with general exercise and physical activity, visit Essex Wellbeing Service and self-refer or click on Self Help for advice on exercises for specific joints in the body.
It is safe and important that you remain active with joint hypermobility.
Fibromyalgia is a long-term condition that causes pain and tiredness all over your body rather than specifically in your joints. It is estimated to that nearly 3 million people in the UK have fibromyalgia and it affects women more than men.
The condition is NOT a type of arthritis and there are is no damage to your joints, bones or muscles. It’s thought to be caused by an oversensitive pain protective system resulting in changes to how the brain and spinal cord process information.
Click Here for some essential information on fibromyalgia, including what you can do to help yourself.
As well as experiencing widespread pains throughout your body, fibromyalgia is linked to poor sleep, lack of concentration, extreme fatigue and low mood. Many symptoms of fibromyalgia are similar to those of other conditions that usually need to be investigated and ruled out first by your GP or specialist before the diagnosis can be made.
Fibromyalgia should be treated as a persistent or chronic pain problem so managing pain effectively is essential to help you cope better with the condition including physical and psychological therapies as well as drug treatments occasionally. Click on Persistent Pain for further help on understanding pain better, changing the way you approach it and establishing what support you may need.
For more information on symptoms, causes, diagnosis and treatment of fibromyalgia – Click Here.
This booklet provides further information and answers to your questions about fibromyalgia.
Remaining active and graded exercise is important if you have fibromyalgia. If you need some help with general exercise, physical activity or support living with this long-term condition, visit Essex Wellbeing Service and self-refer.
If you feel your mental health is being affected by your fibromyalgia, visit NHS Website – Health in Mind for further help and support including online self-referral to access talking therapy treatments if you live in the appropriate Essex region.
Self help
Evidence has shown that people who understand their Musculoskeletal health problem and take an active involvement to help themselves have a much better outcome.
Here are some really helpful leaflets, videos, exercises and useful links to other websites that have been approved by our physiotherapists so that you can start getting better with your multiple joint pain today!
This information is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment if required. All content is for general information purposes only.
Leaflets
Videos
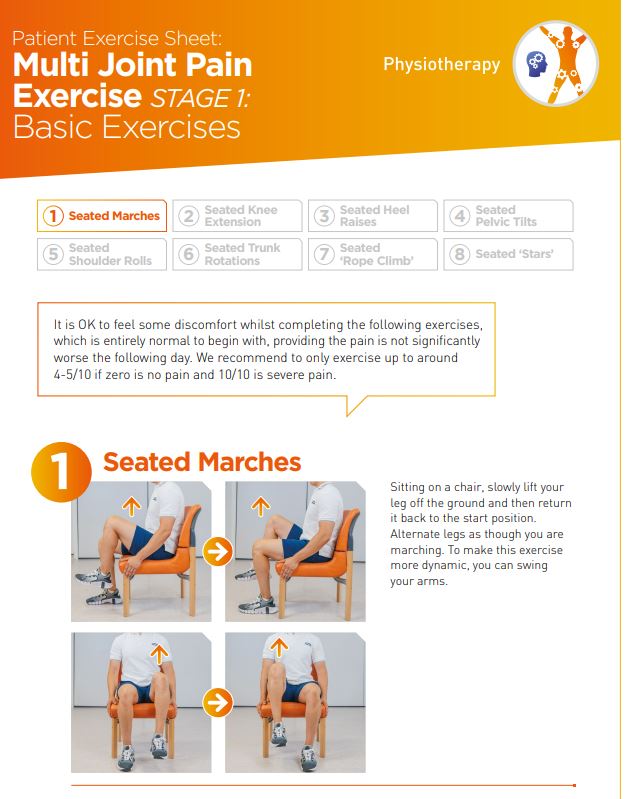
Exercises
Useful Links
- Versus Arthritis is the largest charity in the UK dedicated to caring and supporting people with arthritis
- Advice, tips and tools to help you make the best choices about your health and wellbeing and improve your joint pains
- Further information on the causes of single and multiple joint pain
- Overview of the different types of arthritis and how to live better with the condition
- Arthritis Action is a UK-based charity offering hands-on, practical help for people with arthritis
- Learn more about living well with osteoarthritis
- Educational videos delivered by NHS healthcare professionals on various Rheumatology Conditions and Medications used for these conditions
- Information and support for people with rheumatoid arthritis and their families, friends and carers
- Read more about ankylosing spondylitis, also known as axial spondyloarthritis, including ways to help yourself and support available
- UK Gout Society is a charity that provides basic information to people living with gout, their families, friends and carers
- Information on juvenile idiopathic arthritis, what it is, how it’s managed and living with the condition.
- Resource where people with joint hypermobility syndrome support each other using a positive self-management model
- Overview of fibromyalgia including effective long-term self-help strategies
- If you feel your mental health is being affected by your multiple joint pain, visit NHS Website – Health in Mind for further help and support including online self-referral if you require access to talking therapy treatments and live in the appropriate Essex region
Further Support
If your multiple joint pain is still not improving despite following the advice and guidance provided on the website for up to 6 weeks, you may require further help and support from your GP and other healthcare professionals if necessary.
You should see your GP if you suspect you have any of these types of multiple joint pain which are causing ongoing symptoms and functional problems so that they can confirm the diagnosis, which may require further investigations including specific blood tests, and offer any appropriate treatment required.
Contact your GP for advice if you have any of the following symptoms that have started around the same time as your multiple joint pain:
- Fever or chills
- Tiredness and a lack of energy
- Poor appetite
- Weight loss
- General feeling of being unwell
- Dry or sore eyes
- Chest or abdominal pains
- Diarrhoea for more than seven days
- Rash
FAQs